KAISER PERMANENTE Utilization Management and Resource Management Program
Specifications:
- Utilization Management and Resource Management Program
- Compliance with California’s Health and Safety Code (H&SC)/Knox-Keene Health Care Service Plan Act
- Adherence to managed care plan NCQA accreditation, CMS, DMHC, and DHCS standards
- Data collection for compliance with state and federal regulations
- Regular Member and practitioner satisfaction surveys
Product Usage Instructions
- Utilization Management and Resource Management Overview:
The Utilization Management (UM) and Resource Management (RM) program ensures compliance with statutory requirements and accreditation standards. Data collection and surveys help identify areas for improvement in care. - Medical Appropriateness:
Prior authorization is required for certain services except in emergencies. – Plan Physicians offer various types of care, including specialty care. – Outside referrals may be made when necessary services are not available within the Plan. - Authorization of Services:
Prior authorization is needed for inpatient and outpatient services covered by the Member’s plan. – Providers must render authorized services before the expiration date mentioned in the communication.
FAQ:
- Q: When is prior authorization required?
A: Prior authorization is required for certain healthcare services except in emergencies. - Q: How can I check the authorization status?
A: Contact MSCC for assistance with administrative and patient issues or call the number listed on the Authorization form for Referral Questions.
Overview
Overview of Utilization Management and Resource Management Program
KFHP, KFH, and TPMG share responsibility for Utilization Management (UM) and Resource Management (RM). KFHP, KFH, and TPMG work together to provide and coordinate RM through retrospective monitoring, analysis, and review of the utilization of resources for a full range of outpatient and inpatient services delivered to our Members by physicians, hospitals, and other healthcare practitioners and providers. RM does not affect service authorization. KP does, however, incorporate the utilization of services rendered by Providers into the data sets we study through RM.
UM is a process used by KP for a select number of healthcare services requested by the treating provider to determine whether or not the requested service is medically indicated and appropriate. If the requested service is medically indicated and appropriate, the service is authorized and the Member will receive the services in a clinically appropriate place consistent with the terms of the Member’s health coverage. UM, activities and functions include the prospective (before authorization), retrospective (claims review), or concurrent review (while Member is receiving care) of health care services. The decisions to approve, modify, delay, or deny the request are based in whole or in part on appropriateness and indication. The determination of whether a service is medically indicated and appropriate is based upon criteria developed with the participation of actively practicing physicians. The criteria are consistent with sound clinical principles and processes reviewed and approved annually and updated as needed.
KP’s utilization review program and processes follow statutory requirements contained in California’s Health and Safety Code (H&SC)/Knox-Keene Health Care Service Plan Act. In addition, the UM process adheres to managed care plan NCQA accreditation, CMS, DMHC, and DHCS standards.
Data Collection and Surveys
- KP collects UM data to comply with state and federal regulations and accreditation requirements. Evaluation of UM data identifies areas for improvement in inpatient and outpatient care.
- KP conducts Member and practitioner satisfaction surveys on a regular basis to identify patterns, trends, and opportunities for performance improvement related to UM processes.
- UM staff also monitor and collect information about the appropriateness and indication of health care services and benefits-based coverage decisions. Appropriately licensed healthcare professionals supervise all UM and RM processes.
Medical Appropriateness
- In making UM decisions, KP relies on written criteria of appropriateness and indication developed in collaboration with practicing physicians. The criteria are based on sound clinical evidence and developed by established policies and compliance with statutory requirements. Only appropriately licensed healthcare professionals make UM decisions to deny, delay, or modify provider-requested services. All UM decisions are communicated in writing to the requesting physician. Each UM denial notification includes a clinical explanation of the reasons for the decision and the criteria or guidelines used to determine appropriateness and indication of care or services. UM decisions are never based on financial incentives or rewards to the reviewing UM physician.
- Plan Physicians designated as UM reviewers may be physician leaders for Outside Referral Services, physician experts and specialists (e.g., DME), and/or members of physician specialty boards or committees (e.g., Organ Transplant, Autism Services). These physicians have current, unrestricted licenses to practice medicine in California and have appropriate education, training, and clinical experience related to the requested health care service. When necessary, consultation with board-certified physicians in the associated sub-specialty is obtained to make a recommendation concerning a UM decision.
General Information
- Prior authorization is a UM process that is required for certain healthcare services. However, no prior authorization is required for Members seeking emergency care.1
- Plan Physicians offer primary medical, behavioral health, pediatric, and OB-GYN care as well as specialty care. However, Plan Physicians may refer a Member to a non-plan Provider when the Member requires covered services and/or supplies that are not available in the Plan or cannot be provided promptly. The outside referrals process originates at the facility level and the Assistant Physicians-In-Chief (APICs) for Outside Services (Referrals) are responsible for reviewing the appropriateness, indication, and availability of services for which a referral has been requested.
- The request for a referral to a non-Plan provider (Outside Referrals) is subject to prior authorization and managed at the local facility level. Once the referral is submitted, it is reviewed by the facility and the APICs for Outside Referrals to determine whether services are available in the Plan. If not, the APIC will confirm appropriateness and indication with the requesting physician or designated specialist based on their clinical judgment and approve the Outside Referral request. Outside Referrals for specific services such as DME, solid organ and bone marrow transplants, and behavioral health treatment for autism spectrum disorder are subject to prior authorization using specific UM criteria. These healthcare service requests are reviewed for appropriateness and indication by specialty boards and physician experts.
- When KP approves Referrals for a Member, the outside provider receives a written Authorization for Medical Care communication, which details the name of the referring Plan Physician, the level and scope of services authorized, and the number of visits and/or duration of treatment. The Member receives a letter that indicates a referral has been approved for the Member to see a specific outside Provider. Any additional services beyond the scope of the authorization must have prior approval. To receive approval for additional services, the outside Provider must contact the referring physician.
- Authorized services must be rendered before the authorization expires or before notice from KP that the authorization is canceled. The expiration date is noted in the Authorization for Medical Care communication and/or the Patient Transfer Referral form.
- For assistance in resolving administrative and patient issues (e.g., member benefits and eligibility), please contact MSCC. For authorization status or questions about the referral process, please call the number for Referral Questions listed on the Authorization form.
1An emergency medical condition means (i) as defined in California Health & Safety Code 1317.1 for Members subject to the Knox-Keene Act (a) a medical condition manifesting itself by acute symptoms of sufficient severity (including severe pain) such that the absence of immediate medical attention could reasonably be expected to result in placing the Member’s health in serious jeopardy, or serious impairment to bodily functions, or serious dysfunction of any bodily organ or part; or (b) a mental disorder that manifests itself by acute symptoms of sufficient severity that it renders the Member an immediate danger to themselves or others, or immediately unable to provide for, or utilize, food, shelter or clothing due to the mental disorder; or (ii) as otherwise defined by applicable law (including but not limited to the Emergency Medical Treatment and Active Labor Act (EMTALA) in 42 United States Code 1395dd and its implementing regulations)
Prior authorization is required as a condition of payment for any inpatient and outpatient services (excluding emergency services) that are otherwise covered by a Member’s benefit plan. In the event additional services were rendered to the Member without prior authorization (other than investigational or experimental therapies or other non-covered services), the Provider will be paid for the provision of such services in a licensed acute care hospital if the services were related to services that were previously authorized and when all the following conditions are met:
- The services were medically necessary at the time they were provided;
- The services were provided after KP’s normal business hours; and
- A system that provides for the availability of a KP representative or an alternative means of contact through an electronic system, including voice mail or electronic mail, was not available. For example, KP could not/did not respond to a request for authorization within 30 minutes after the request was made.
NOTE: Authorization from KP is required even when KP is the secondary payor.
Hospital Admissions Other Than Emergency Services
A Plan Physician may refer a Member to a hospital for admission without prior UM review. The RM staff conducts an initial review within 24 hours of admission using hospital stay criteria to confirm the appropriate level of care and the provision of services. KP Referral Patient Care Coordinator Case Managers (PCC-CMs) are responsible for notifying the treating physician of the review outcome.
Admission to Skilled Nursing Facility (SNF)
- If the level of care is an issue or other services better meet the clinical needs of the Member, a PCC-CM will notify the ordering/treating physician to discuss alternative treatment plans, including admission to an SNF.
- A Plan Physician may refer a Member for a skilled level of care at an SNF. The service authorization is managed by a PCC-CM and includes a description of specific, approved therapies and other medically necessary skilled nursing services per Medicare Guidelines.
- The initial skilled care authorizations are based on the Member’s medical needs at the time of admission, the Member’s benefits, and eligibility status. The Member is informed by a PCC-CM as to what their authorized and anticipated length of stay may be. The Member’s clinical condition and physician assessment will inform the final determination during the Member’s course of care in the SNF.
- The SNF may request an extension of authorization for continued stay. This request is submitted to the SNF Care Coordinator. This request is reviewed for appropriateness and indication and may be denied when the patient does not meet skilled services criteria per Medicare Guidelines. The SNF Care Coordinator conducts telephonic or onsite reviews at least weekly to evaluate the Member’s clinical status, and level of care needs, and to determine if continuation of the authorization is appropriate. Based on the Member’s skilled care needs and benefit eligibility, more SNF days may be approved. If additional days are authorized, the SNF will receive written authorization from KP.
Other services associated with the SNF stay are authorized when either the Member’s Plan Physician or other KP-designated specialist expressly orders such services. These services may include, but are not limited to, the following items:
- Laboratory and radiology services
- Special supplies or DME
- Ambulance transport (when Member meets criteria)
Authorization Numbers are Required for Payment
- KP requires that authorization numbers be included on all claims submitted by not only SNFs but all ancillary providers that provide services to KP Members (e.g., mobile radiology vendors).
- These authorization numbers must be provided by the SNF to the rendering ancillary services provider, preferably at the time of service. Because authorization numbers may change, the authorization number reported on the claim must be valid for the date of service provided. Please note that the correct authorization number for the ancillary service providers may not be the latest authorization issued to the SNF.
- It is the responsibility of the SNF to provide the correct authorization number(s) to all ancillary service providers at the time of service. If SNF personnel are not sure of the correct authorization number, please contact KP’s SNF Care Coordinator for confirmation.
Home Health/Hospice Services
Home health and hospice services require prior authorization from KP. Both home health and hospice services must meet the following criteria to be approved:
- A Plan Physician must order and direct the requests for home health and hospice services
- The patient is an eligible Member
- Services are provided by benefit guidelines
- The patient requires care in the patient’s place of residence. Any place that the patient is using as a home is considered the patient’s residence
- The home environment is a safe and appropriate setting to meet the patient’s needs and provide home health or hospice services
- There is a reasonable expectation that the patient’s clinical needs can be met by the Provider
Home Health-Specific Criteria
Prior authorization is required for home health care services. Criteria for coverage include:
- The services are medically necessary for the Member’s clinical condition
- The patient is homebound, which is defined as an inability to leave home without the aid of supportive devices, special transportation, or the assistance of another person.
- A patient may be considered homebound if absences from the home are infrequent and of short distances. A patient is not considered homebound if lack of transportation or inability to drive is the reason for being confined to the home
- The patient and/or caregiver(s) are willing to participate in the plan of care and work toward specific treatment goals
Hospice Care Criteria
Prior authorization is required for Hospice Care. Criteria for coverage include:
- The patient is certified as being terminally ill and meets the criteria of the benefit guidelines for hospice services.
Durable Medical Equipment (DME)/ Prosthetics and Orthotics (P&O)
Prior Authorization is required for DME and P&O. KP evaluates authorization requests for appropriateness based on, but not limited to:
- The Member’s care needs
- The application of specific benefit guidelines
- For further information on ordering DME, please contact the assigned KP Case Manager
Psychiatric Hospital Services Other Than Emergency Services
Plan Physicians admit Members to psychiatric facilities by contacting the KP Psychiatry/ Call Center Referral Coordinator. Once a bed has been secured, KP will generate an authorization confirmation for the facility Provider.
Non-Emergent Transportation
To serve our Members and coordinate care with our Providers, KP has a 24-hour, 7-day-per-week, centralized medical transportation department called the “HUB”, to coordinate and schedule non-emergency medical transportation. The HUB can be reached at 800-438-7404.
Non-Emergency Medical Transport (Gurney Van/Wheelchair Van)
Non-Emergency Medical Transport services require prior authorization from KP. Providers must call the KP HUB to request non-emergency medical transportation.
- Non-emergency medical transportation may or may not be a covered benefit for the Member. Payment may be denied for non-emergency medical transportation unless KP issued a prior authorization and the transportation was coordinated through the HUB.
Non-Emergency Ambulance Transportation
- Non-emergency ambulance transportation must be authorized and coordinated by the KP HUB. If a Member requires non-emergency ambulance transportation to a KP Medical Center or any other location designated by KP, Providers may contact KP to arrange the transportation of the Member through the HUB. Providers should not contact any ambulance company directly to arrange an authorized non-emergency ambulance transportation of a Member.
- Non-emergency ambulance transportation may or may not be a covered benefit for the Member. Payment may be denied for ambulance transport of a Member unless KP issued a prior authorization and the transportation was coordinated through the HUB.
Transfers to a KP Medical Center
- If, due to a change in a Member’s condition, the Member requires a more intensive level of care than your facility can provide, you can request a transfer of the Member to a KP Medical Center. The Care Coordinator or designee will arrange the appropriate transportation through KP’s medical transportation HUB.
- Transfers to a KP Medical Center should be made by the facility after verbal communication with the appropriate KP staff, such as a TPMG SNF physician or the Emergency Department physician. Contact a Care Coordinator for a current list of telephone numbers for emergency department transfers.
- If a Member is sent to the Emergency Department via a 911 ambulance and it is later determined by KP that the 911 ambulance transport or emergency department visit was not medically necessary, KP may not be obligated to pay for the ambulance transport.
Required Information for Transfers to KP
Please send the following written information to the Member:
- Name of Member’s contact person (family member or authorized representative) and telephone number
- Completed inter-facility transfer form
- Brief history (history and physical, discharge summary, and/or admit note)
- Current medical status, including presenting problem, current medications, and vital signs
- A copy of the patient’s Advance Directive/Physician Orders for Life Sustaining Treatment (POLST)
- Any other pertinent medical information, i.e., lab/x-ray
If the Member is to return to the originating facility, KP will provide the following written information:
- Diagnosis (admitting and discharge)
- Medications given; new medications ordered
- Labs and x-rays performed
- Treatment(s) given
- Recommendations for future treatment; new orders
Visiting Member Guidelines
- KP Members who access routine and specialty health services while they are visiting another KP region are referred to as “visiting Members.” Certain KP health benefit plans allow Members to receive non-urgent and non-emergent care while traveling in other KP regions. The KP region being visited by the Member is referred to as the “Host” region, and the region where a Member is enrolled is their “Home” region.
- Visiting Members to KPNC are subject to the UM and prior authorization requirements outlined in the visiting Member’s coverage documents.
Your first step when a visiting Member has been referred to you by KP:
- Review the Member’s Health ID Card. The KP “Home” region is displayed on the face of the card. Confirm the Member’s “Home” region MRN.
- Verify “Home” region benefits, eligibility, and cost-share via Online Affiliate. or by calling the “Home” region’s Member Services Contact Center (number provided on the identification card).
- If the Member does not have their Health ID Card, call the Member’s “Home” region at the number provided in the table at the end of this section.
- Services are covered according to the Member’s contract benefits, which may be subject to exclusions as a visiting Member. Providers should identify the Member as a visiting Member when verifying benefits with the “Home” region.
The KP MRN identified on the KP authorization will not match the MRN on the visiting Member’s KP ID card:
- Visiting Members require KPNC to establish a “Host” MRN for all authorizations. * When communicating with KPNC about authorization matters, reference the “Host” MRN. The “Home” MRN should only be used on claims, as detailed.
- Contractors should always verify any Member’s identity by requesting a picture ID before rendering services.
EXCEPTION: for DME authorizations, contact the “Home” region at the number below.
| Regional Member Services Call Centers | |
| Northern California | (800)-464-4000 |
| Southern California | (800)-464-4000 |
| Colorado | 800-632-9700 |
| Georgia | 888-865-5813 |
| Hawaii | 800-966-5955 |
| Mid-Atlantic | 800-777-7902 |
| Northwest | 800-813-2000 |
| Washington
(formerly Group Health) |
888-901-4636 |
Emergency Admissions and Services; Hospital Repatriation Policy
Consistent with applicable law, KP Members are covered for emergency care to stabilize their clinical condition. An emergency medical condition means (i) as defined in California Health & Safety Code 1317.1 for Knox-Keene Members (a) a medical condition manifesting itself by acute symptoms of sufficient severity (including severe pain) such that the absence of immediate medical attention could reasonably be expected to result in placing the Member’s health in serious jeopardy, or serious impairment to bodily functions, or serious dysfunction of any bodily organ or part or (b) a mental disorder that manifests itself by acute symptoms of sufficient severity that it renders the Member an immediate danger to themselves or others, or immediately unable to provide for, or utilize, food, shelter, or clothing due to the mental disorder; or (ii) as otherwise defined by applicable law (including but not limited to Emergency Medical Treatment and Active Labor Act (EMTALA) in 42 United States Code 1395dd and its implementing regulations).
Emergency Services to screen and stabilize a Member suffering from an emergency medical condition as defined above do not require prior authorization.
Emergency Services
- If Emergency Services are provided to screen and stabilize a patient in California, they are covered in situations when an emergency condition (as defined above) existed
- Once a patient is stabilized, the treating physician is required to communicate with KP for approval to provide further care or to effect transfer
Emergency Claim
The following circumstances will be considered when the bill is processed for payment:
- Whether services and supplies are covered under the Member’s benefit plan
- Members have varying benefit plans, and some benefit plans may not cover continuing or follow-up treatment at a non-plan facility. Therefore, the Provider should contact KP’s Emergency Prospective Review Program (EPRP) before furnishing post-stabilization services.
Emergency Prospective Review Program (EPRP)
EPRP provides a statewide notification system relating to emergency services for Members. Prior authorization is not required for emergency admissions. Post-stabilization care at a non-plan facility must have prior authorization by EPRP. EPRP must be contacted before a stabilized Member’s admission to a non-Plan facility. KP may arrange for medically necessary continued hospitalization at the facility or transfer the Member to another hospital after the Member is stabilized.
When a Member presents in an emergency room for treatment, we expect the Provider to triage and treat the Member by EMTALA requirements, and to contact EPRP once the Member has been stabilized or stabilizing care has been initiated.* The Provider may contact EPRP at any time, including before stabilization to the extent legally and clinically appropriate, to receive relevant patient-specific medical history information which may assist the Provider in its stabilization efforts and any subsequent post-stabilization care. EPRP has access to Member medical history, including recent test results, which can help expedite diagnosis and inform further care.
Under the EMTALA regulations Providers may, but are not required to, contact EPRP once stabilizing care has been initiated but before the patient’s actual stabilization if such contact will not delay necessary care or otherwise harm the patient.
EPRP
800-447-3777 Available 7 days a week 24 hours a day
EPRP is available 24 hours a day, every day of the year and provides:
- Access to clinical information to help the Provider in evaluating a Member’s condition and to enable our physicians and the treating physicians at the facility to quickly determine the appropriate treatment for the Member
- Emergency physician-to-emergency physician discussion regarding a Member’s condition
- Authorization of post-stabilization care or assistance with making appropriate alternative care arrangements
Post-Stabilization Care
If there is mutual agreement at the time of the phone call as to the provision of post-stabilization services, EPRP will authorize the Provider to provide the agreed services and issue a confirming authorization number. If requested, EPRP will also provide, by fax or other electronic means, a written confirmation of the services authorized and the confirmation number. KP will send a copy of the authorization to the facility’s business office within 24 hours of the authorization decision. This authorization number must be included with the claim for payment for the authorized services. The authorization number is required for payment, along with all reasonably relevant information relating to the post-stabilization services on the claim submission consistent with the information provided to EPRP as the basis for the authorization.
- EPRP must have confirmed that the Member was eligible for and had benefit coverage for the authorized post-stabilization services provided before the provision of post-stabilization services.
- If EPRP authorizes the admission of a clinically stable Member to the facility, KP’s Outside Services Case Manager will follow that Member’s care in the facility until discharge or transfer.
- EPRP may request that the Member be transferred to a KP-designated facility for continuing care or EPRP may authorize certain post-stabilization services in your facility. In many cases, such post-stabilization services will be rendered under the management of a physician who is a member of your facility’s medical staff and who has contracted with KP to manage the care of our Members being treated in community hospitals.
- EPRP may deny authorization for some or all post-stabilization services. The verbal denial of authorization will be confirmed in writing. If EPRP denies authorization for requested post-stabilization care, KP shall not have financial responsibility for services if the Provider nonetheless chooses to provide the care. If the Member insists on receiving such unauthorized post-stabilization care from the facility, we strongly recommend that the facility require that the Member sign a financial responsibility form acknowledging and accepting his or her sole financial liability for the cost of the unauthorized post-stabilization care and/or services.
- If the Member is admitted to the facility as part of the stabilizing process and the facility has not yet been in contact with EPRP, the facility must contact the local Outside Services Case Manager at the appropriate number (see the contact information of this Provider Manual) to discuss authorization for continued admission as well as any additional appropriate post-stabilization care once the Member’s condition is stabilized.
Concurrent Review
- The Northern California Outside Utilization Resource Services (NCAL OURS) Office and Plan Physicians will conduct concurrent reviews in collaboration with facilities. The review may be done telephonically or on site in accordance with the facility’s protocols and KP’s onsite review policy and procedure, as applicable.
- Prior authorization is not required for out-of-plan hospitals rendering screening and stabilizing services in California. Outside Services Case Managers work with physicians to concurrently evaluate the appropriateness and indication of out-of-plan care. KP will facilitate transfer and coordinate the continuing care needed by Members who are determined to be clinically stable for transfer to a KFH or contracting hospital.
- When utilization problems are identified, KP will work with the facility to develop and implement protocols that are intended to improve the provision of services for our Members. A joint monitoring process will be established to observe for continued improvement and cooperation.
NCAL OURS and the Providers collaborate on concurrent review activities that include, but are not limited to:
- monitoring the length of stay/visits
- providing day/service authorization, recertification, justification
- attending patient care conferences and rehabilitation meetings
- utilizing community benchmarking for admissions and average length of stay (ALOS)
- setting patient goals for Members
- conducting visits or telephonic reports, as needed
- developing care plans
Case Management Hub Contact Information
The specific contact information for NCAL OURS is as follows:
- Main Phone Line: 925-926-7303
- Toll-free phone line: 1-888-859-0880
- eFax: 1-877-327-3370
The NCAL OURS office is located in Walnut Creek, providing support for all Northern California KP Members admitted in any non-KP hospital, including those Members admitted out of the KP service area and out of the country.
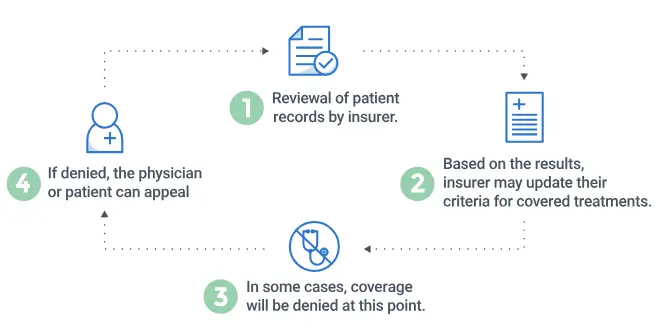
Denials and Provider Appeals
- Information about a denial or the appeal procedures is available via Online Affiliate or by contacting the Coverage Decision Support Unit (CDSU) or Member Services Contact Center (MSCC). Please refer to the written denial notice for applicable contact information or contact MSCC.
- When a denial is made, the Provider is sent a UM denial letter accompanied by the name and direct telephone number of the decision-maker. All decisions concerning appropriateness and indication are made by physicians or licensed clinicians (as appropriate for behavioral health services). Physician UM decision-makers include but are not limited to, DME physician champions, APICs for Outside Services, Pediatric Developmental Disabilities Office, other board-certified physicians, or behavioral health practitioners.
- If the physician or behavioral health practitioner does not agree with a decision concerning appropriateness and indication, the Provider may contact the UM decision-maker on the cover page of the letter or the Physician-in-Chief for discussion at the local facility. Providers may also contact the issuing department that is identified in the letter for additional information.
Discharge Planning
- Providers such as hospitals and inpatient psychiatric facilities are expected to provide discharge planning services for Members and to cooperate with KP to ensure timely and appropriate discharge when the treating physician determines that the member no longer needs acute inpatient-level care.
- Providers should designate staff to provide proactive, ongoing discharge planning. Discharge planning services should begin upon the Member’s admission and be completed by the medically appropriate discharge date. The Provider’s discharge planner must be able to identify barriers to discharge and determine an estimated date of discharge. Upon request by KP, Providers will submit documentation of the discharge planning process.
- The Provider’s discharge planner, in consultation with the Care Coordinator, will arrange and coordinate transportation, DME, follow-up appointments, appropriate referrals to community services, and any other services requested by KP.
- The Provider must request prior authorization for medically necessary follow-up care after discharge.
UM Information
To facilitate KP UM oversight, the Provider may be requested to provide information to the KP UM staff concerning the Provider’s facility. Such additional information may include, but is not limited to, the following data:
- Number of inpatient admissions
- Number of inpatient readmissions within the previous 7 days
- Number of emergency department admissions
- Type and number of procedures performed
- Number of consults
- Number of deceased Members
- Number of autopsies
- ALOS
- Quality Assurance/Peer Review Process
- Number of cases reviewed
- Final action taken for each case reviewed
- Committee Membership (participation as it pertains to Members and only by the terms of your contract)
- Utilization of psychopharmacological agents
- Other relevant information KP may request
Case Management
- Care Coordinators work with treating Providers to develop and implement plans of care for acutely ill, chronically ill, or injured Members. KP case management staff may include nurses and social workers, who assist in arranging care in the most appropriate setting and help coordinate other resources and services.
- The PCP continues to be responsible for managing the Member’s overall care. It is the Provider’s responsibility to send reports to the referring physician, including the PCP, of any consultation with, or treatment rendered to, the Member. This includes any requests for authorization or Member’s inclusion in a case management program.
Clinical Practice Guidelines
Clinical Practice Guidelines (CPGs)
- Clinical Practice Guidelines (CPGs) are clinical references used to educate and support clinical decisions by practitioners at the point of care in the provision of acute, chronic, and behavioral health services. The use of CPGs by practitioners is discretionary. However, CPGs can assist Providers in providing Members with evidence-based care that is consistent with professionally recognized standards of care.
- The development of CPGs is determined and prioritized according to established criteria, which include several patients affected by a particular condition/need, quality of care concerns and excessive clinical practice variation, regulatory issues, payor interests, cost, operational needs, leadership mandates, and prerogatives.
- Physicians and other practitioners are involved in the identification of CPG topics, as well as the development, review, and endorsement of all CPGs. The CPG team includes a core, multi-disciplinary group of physicians representing the medical specialties most affected by the CPG topic, as well as health educators, pharmacists, or other medical professionals.
- The CPGs are sponsored and approved by one or more Clinical Chiefs groups, as well as by the Guidelines Medical Director. Established guidelines are routinely reviewed and updated. CPGs are available by contacting MSCC or the referring Plan Physician.
Pharmacy Services/Drug Formulary
KP has developed a quality, cost-effective pharmaceutical program that includes therapeutics and formulary management. The Regional Pharmacy and Therapeutics (P&T) Committee reviews and promotes the use of the safest, most effective, and cost-effective drug therapies, and shares “Best Practices” with all KP Regions. The Regional P&T Committee’s Formulary evaluation process is used to develop the applicable KP Drug Formulary (Formulary) for use by KP practitioners. Contracted practitioners are encouraged to use and refer to the Regional Drug Formulary when prescribing medication for Members (available at http://kp.org/formulary). Drug Coverage and Benefit policies can be found at: https://kpnortherncal.policytech.com/ under the section, Pharmacy Policies: Drug Coverage Benefits.
- For KP Medi-Cal Members without an alternate, primary coverage, medically necessary drugs, supplies, and supplements are covered by DHCS, not KP. Coverage is based on the DHCS Contract Drug List guidelines and Medi-Cal coverage criteria. The DHCS Drug Formulary, called the Contract Drug List, can be accessed online at: https://medi-calrx.dhcs.ca.gov/home/cdl/.
Pharmacy Benefits
Pharmacy services are available for Members who have benefit plans that provide coverage for a prescription drug program. For information on specific member benefit plans, please contact MSCC.
Filling Prescriptions
- The Formulary can be accessed online in a searchable format. It provides the list of drugs approved for general use by prescribing practitioners. For access to the online version of the Formulary on the Internet or to request a paper copy, please refer to the instructions at the end of this section.
- KP pharmacies do not cover prescriptions written by non-Plan Physicians unless authorization for care by that non-Plan Physician has been issued. Please remind Members they must bring a copy of their authorizations to the KP pharmacy when filling the prescription. In limited circumstances, members may have a benefit plan design that covers prescriptions from non-KP Providers, such as for psychotropic drugs or IVF medications.
- Practitioners are expected to prescribe drugs included in the Formulary unless at least one of the exceptions listed under “Prescribing Non-Formulary Drugs” in this section is met. If there is a need to prescribe a non-formulary drug, the exception reason must be indicated on the prescription.
- A Member may request a Formulary exception by contacting their KP physician directly through secure messaging or through the MSCC and will typically receive a response, including the reason for any denial, within 2 Business Days from receipt of the request.
- Members will be responsible for paying the full price of their medication if the drugs requested are (i) non-formulary drugs not required by their health condition, (ii) excluded from coverage (i.e., cosmetic use), or (iii) not prescribed by an authorized or Plan Provider. Any questions should be directed to the MSCC.
Prescribing Non-Formulary Drugs
Non-formulary drugs are those that have not yet been reviewed, and those drugs that have been reviewed but given non-formulary status by the Regional P&T Committee. However, the situations outlined below may allow a non-formulary drug to be covered by the Member’s drug benefit.
- New Members
If needed and the Member’s benefit plan provides, new Members may be covered for an initial supply (up to 100 days for Commercial Members and at least a month’s supply of medication for Medicare Members) of any previously prescribed “non-Formulary” medication to allow the Member time to make an appointment to see a KP provider. If the Member does not see a KP provider within the first 90 days of enrollment, they must pay the full price for any refills of non-formulary medications. - Existing Members
A non-formulary drug may be prescribed for a Member if they have an allergy, intolerance to, or treatment failure with all Formulary alternatives or have a special need that requires the Member to receive a non-formulary drug. For the Member to continue to receive the non-formulary medication covered under their drug benefit, the exception reason must be provided on the prescription.
NOTE:
Generally, non-formulary drugs are not stocked at KP pharmacies. Therefore, before prescribing a non-formulary drug, call the pharmacy to verify the drug is available at that site. The KP Formulary may be found at http://kp.org/formulary.
- Pharmacies
KP pharmacies provide a variety of services including: filling new prescriptions, transferring prescriptions from another pharmacy, and providing refills and medication consultations. - Telephone and Internet Refills
- Members may request refills on their prescriptions, with or without refills remaining, by calling the pharmacy refill number on their prescription label. All telephone requests should be accompanied by the Member’s name, MRN, daytime phone number, prescription number, and credit or debit card information.
- Members may also refill their prescriptions online by accessing the KP Member website at http://www.kp.org/refill.
- Mail Order
- Members with a prescription drug benefit are eligible to use the KP “Prescription by Mail” service. For more information regarding mail order prescriptions please contact the Mail Order Pharmacy at 888-218-6245.
- Only maintenance medications should be ordered for delivery by mail. Acute prescriptions such as antibiotics or pain medications should be obtained through a KP pharmacy to avoid delays in treatment.
- Restricted Use Drugs
Some drugs (i.e., chemotherapy) are restricted to prescribing only by approved KP specialists. Restricted drugs are noted in the Formulary. If you have any questions regarding prescribing restricted drugs, please call the main pharmacy at the local KP facility. - Emergency Situations
- If emergency medication is needed when KP pharmacies are not open, Members may use pharmacies outside of KP. Since the Member will have to pay the full retail price in this situation, they should be instructed to download a claim form on KP.org or to call Member Services at 800-464-4000 (TTY: 711) to obtain a claim form to be reimbursed for the cost of the prescription less any copayments, co-insurance and/or deductibles
(sometimes called Member Cost Share) which may apply. - It is your responsibility to submit itemized claims for services provided to Members in a complete and timely manner by your Agreement, this Provider Manual, and applicable law. KFHP is responsible for the payment of claims by your Agreement. Please note that this Provider Manual does not address the submission of claims for fully insured or self-funded products underwritten or administered by Kaiser Permanente Insurance Company (KPIC).
- If emergency medication is needed when KP pharmacies are not open, Members may use pharmacies outside of KP. Since the Member will have to pay the full retail price in this situation, they should be instructed to download a claim form on KP.org or to call Member Services at 800-464-4000 (TTY: 711) to obtain a claim form to be reimbursed for the cost of the prescription less any copayments, co-insurance and/or deductibles
Documents / Resources
 |
KAISER PERMANENTE Utilization Management and Resource Management Program [pdf] Owner's Manual Utilization Management and Resource Management Program, Management and Resource Management Program, Resource Management Program, Management Program, Program |




